Serotonin Hormone Role in Ejaculation
Serotonin is the key hormone that stabilizes our mood, feelings of well-being, and happiness. This hormone impacts your entire body. It enables brain cells and other nervous system cells to communicate with each other. Serotonin also helps with sleeping, eating, and digestion.
It’s well known that anti-depressants can have sexual side effects. They can lead to problems with:
- Desire
- Arousal
- Ejaculation
- Orgasm
These sexual problems are most associated with the use of two drug classes—selective serotonin reuptake inhibitors (SSRIs) and serotonin-norepinephrine reuptake inhibitors (SNRI)—used to treat depression and other mood disorders.1
:max_bytes(150000):strip_icc():format(webp)/shirtless-worried-man-with-blanket-sitting-on-bed-at-home-1137905752-74449c5bb8d64f99a6993739f1dd68aa.jpg)
Very early on in the development of SSRIs, it was discovered that these medications can cause difficulties with ejaculation. In fact, these medications are actually sometimes prescribed for men who have problems with premature ejaculation.
Why can antidepressants have such profound effects on sexual health, particularly for men? It has nothing to do with mood. Instead, it has to do with the role of serotonin and other neurotransmitters in arousal and ejaculation.
The Biology of Ejaculation
Sex is, in many ways, a function of the mind.
Physical arousal can take place by direct stimulation. It can also take place without any direct stimulation. Sex therapists often recommend “sexy thoughts” as an intervention, because thinking about sex can be a turn on in and of itself.
How does that work? The same way that many thoughts are processed—through the production of various neurotransmitters. That’s how nerve cells communicate with each other. They release and respond to neurotransmitters, including:
- Serotonin
- Norepinephrine
- Dopamine
Much of our understanding of the role of neurotransmitters and brain structures in arousal and orgasm comes from animal research. However, there have been human studies as well.
Through research, scientists have learned that several areas of the brain are associated with male sexual function.
The medial preoptic area (MPOA) of the hypothalamus is central to the sexual response. This is where sexual stimuli from various parts of the body come together for processing.
The brain then sends signals down the spinal cord that cause the body to become aroused and then orgasm. Parts of the amygdala and the parietal cortex are also important in the control of ejaculation.
Role of Neurotransmitters
Neurotransmitters are the mechanism for these signals. Studies in rats have shown that it is possible to cause rats to orgasm just by activating certain neurotransmitter receptors in the brain.
In humans, serotonin is the neurotransmitter most clearly associated with ejaculation. SSRIs work by preventing cells from reabsorbing (reuptaking) serotonin. This means that signals caused by serotonin are extended, lasting for a longer period of time.
The chronic use of SSRI antidepressants has been shown to extend the time between erection and ejaculation in men. This is why they are sometimes prescribed as a treatment for premature ejaculation.
Interestingly, studies in rats have shown that where the serotonin is changed its effects. When serotonin is injected into some parts of the rat brain, it causes a delay in ejaculation. In other areas of the brain, it causes ejaculation to take place.
Dopamine also plays a role in ejaculation, although its role has not been as thoroughly explored as that of serotonin.
Studies in rats suggest that dopamine stimulation can cause ejaculation to take place. In humans, there is also research to support this.4
People with schizophrenia who are treated with antipsychotic drugs that block a particular type of dopamine receptor (D2-like receptors) are likely to find it difficult, or impossible, to ejaculate. Those same drugs have been tested in men with premature ejaculation.
Similar to SSRIs, antipsychotics seem to extend the time between arousal and ejaculation. In addition, there is a small amount of data suggesting that mutations in dopamine transporters may make some men more likely to experience premature ejaculation.
Phases of Ejaculation
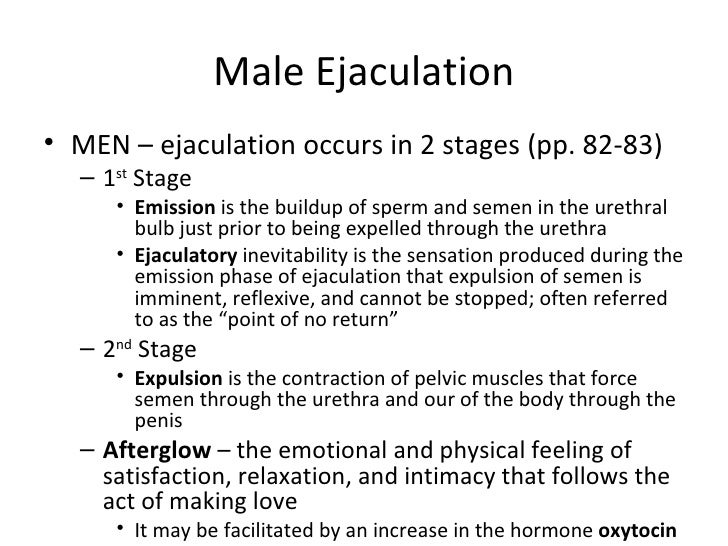
Ejaculation is defined as the forceful propulsion of semen from the body. It takes place in two phases.
The first phase is referred to as emission. That is when the various components of the semen, including sperm, are secreted from various glands and organs.
The second phase is expulsion. That is when intense contractions of the muscles in the genital region cause semen to be pushed out of the penis.
Of note, some men who have had certain types of prostate cancer surgery may experience “dry” ejaculation. This is because their bodies no longer produce the fluid components of semen.
Approximately one-third of seminal fluid comes from the prostate. Other glands that contribute to seminal fluid production can also be affected by cancer surgeries.6
The term “orgasm” is often used synonymously with ejaculation even though they are not the same thing. Although orgasm (characterized by feelings of intense pleasure) often takes place at the time of ejaculation, it can occur without ejaculation.
Some men who are multi-orgasmic may have multiple orgasms with only one ejaculation. Other men are not able to ejaculate at all. This condition is known as anejaculation.
Erection vs. Ejaculation
It is important to note that an erection is not required for ejaculation to occur. Ejaculation without erection is not common, but it is possible.
The most frequent example of this takes place in adolescent boys while they sleep, referred to as nocturnal emissions or “wet dreams.” Nocturnal emissions can occur with or without the presence of an erection.
Ejaculation without erection can also be stimulated using the vibration of the penis in men with certain types of spinal cord injury. This technique is also sometimes used to collect sperm for assisted reproduction procedures.
Though the physiological pathways that lead to erection and ejaculation are related, they are not the same. This is why the PDE-5 inhibitors used to treat erectile dysfunction do not have a significant impact on a man’s ability to ejaculate.
They affect the flow of blood into and out of the penis. They do not affect the release of the components of semen or the muscle contractions of expulsion.






