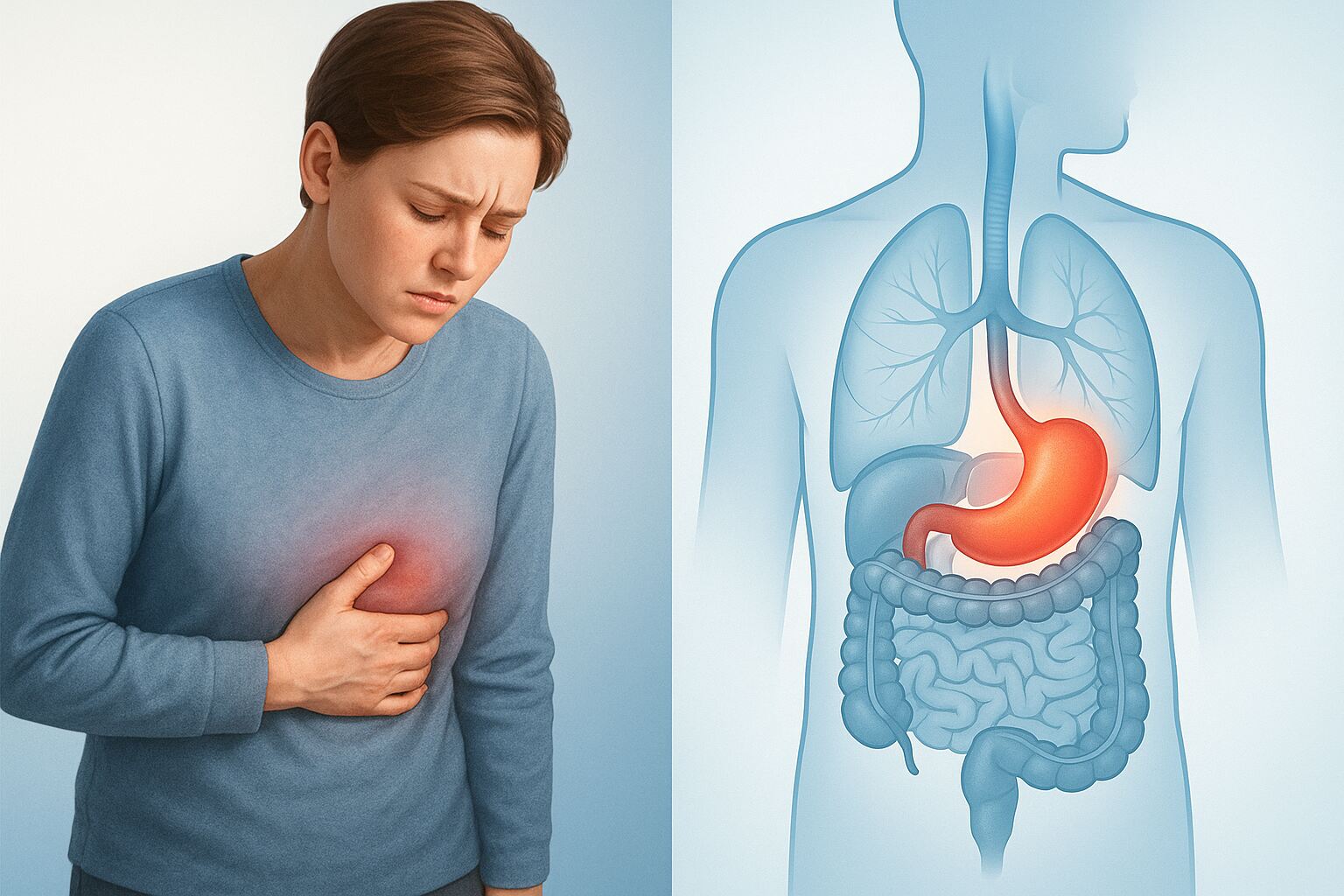
Indigestion is one of those uncomfortable experiences most of us know all too well—that uneasy feeling in your stomach after a meal, the burning sensation in your chest, or that persistent sense of fullness that just won’t go away. Medically known as dyspepsia, indigestion affects approximately 20% of the population and can range from an occasional nuisance to a chronic condition that impacts daily life.
Understanding what causes indigestion and how to manage it effectively can make a significant difference in your comfort and quality of life. This comprehensive guide will help you recognize the symptoms, understand the underlying causes, and discover evidence-based strategies for relief.
What Is Indigestion?
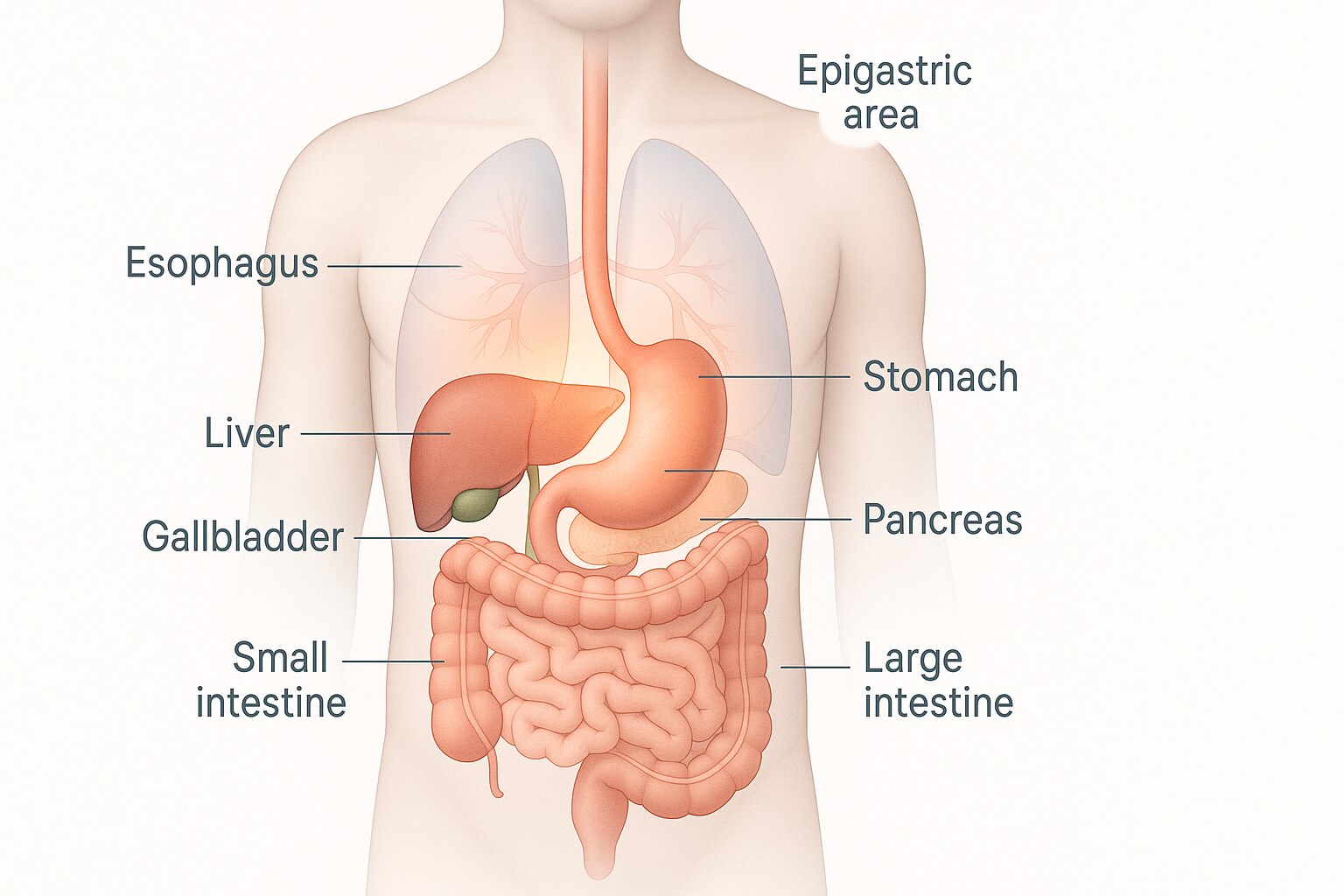
Indigestion, or dyspepsia, refers to pain or discomfort in your upper abdomen—the region that houses your stomach, liver, pancreas, and the first part of your small intestine. It’s important to understand that indigestion is not a disease itself, but rather a collection of symptoms that can result from various causes.
The term “dyspepsia” literally means “impaired digestion,” though interestingly, the symptoms often have little to do with actual digestive function. It normally takes three to five hours for your stomach to digest food before passing it to your small intestine. During this time, your pancreas and gallbladder release enzymes and bile to help break food down — right in the same area where indigestion pain tends to show up.
Recognizing the Symptoms
Indigestion presents itself through a variety of symptoms, which can occur individually or together. Most commonly, these symptoms appear during or shortly after eating:
Primary Symptoms
Early Satiety: Only being able to eat a small amount of food before feeling full. You may find yourself unable to finish meals that would normally satisfy you.
Uncomfortable Fullness: A prolonged sensation of fullness that lasts much longer than it should after eating. This feeling can be accompanied by bloating or distension in the upper abdomen.
Upper Abdominal Pain or Discomfort: Pain ranging from mild to severe in the epigastric region—the area between the bottom of your breastbone and your navel. This discomfort may feel like pressure, aching, or cramping.
Burning Sensation: An uncomfortable heat or burning feeling in the upper abdomen or lower chest. This burning sensation is often related to stomach acid irritating the lining of your digestive tract.
Additional Symptoms
- Bloating and a feeling of tightness in the upper abdomen
- Nausea, with or without vomiting
- Belching or burping
- Occasional heartburn (a burning sensation in your chest)
Indigestion almost always includes burning or pain in your upper belly and feeling like you’re full too soon or for too long after you finish eating.
It’s worth noting that symptoms can vary significantly from person to person. Some people experience indigestion occasionally—perhaps after a particularly rich meal—while others deal with it daily, affecting their eating habits and overall quality of life.
Understanding the Causes
The causes of indigestion are diverse and can range from lifestyle factors to underlying medical conditions. Understanding what triggers your symptoms is the first step toward effective management.
The Role of Stomach Acid
The most common cause of indigestion is stomach acid — especially when there’s too much of it or when it gets where it doesn’t belong. Acid can irritate the lining of your stomach, esophagus or small intestine, causing that familiar burning or painful sensation.
Functional Dyspepsia
Functional dyspepsia is chronic indigestion with no identifiable cause. This condition, also called non-ulcer dyspepsia, accounts for more than 70% of chronic indigestion cases. Healthcare providers diagnose “functional” gastrointestinal disorders when they can’t find a direct cause for your symptoms. This might happen because of the close connection between your gut and brain.
Research suggests several factors may contribute to functional dyspepsia, including visceral hypersensitivity (heightened sensitivity to sensations in your digestive organs), problems with how your stomach relaxes and empties, and the gut-brain connection affecting how you perceive discomfort.
Common Medical Causes
Gastroesophageal Reflux Disease (GERD): A condition where stomach contents regularly flow back into the esophagus, causing irritation and inflammation.
Peptic Ulcers: Open sores that develop on the inner lining of your stomach or the upper portion of your small intestine, most commonly caused by H. pylori bacteria or NSAID use.
Helicobacter pylori Infection: More than 1 in 4 people in the UK become infected with H. pylori at some stage in their lives. This bacteria can infect the stomach lining and is a leading cause of ulcers and gastritis.
Gastritis: Inflammation of the stomach lining that can result from infection, medications, or stress.

Lifestyle and Dietary Factors
Many cases of occasional indigestion stem from how and what we eat:
- Eating too much or too quickly
- Consuming fatty, greasy, or spicy foods
- Eating during stressful situations
- Lying down immediately after eating
- Consuming caffeine, alcohol, or carbonated beverages
- Smoking tobacco
- Swallowing a lot of air when you eat or drink may increase the symptoms of burping and bloating.
Medication Side Effects
Many drugs are frequently associated with indigestion, for example, nonsteroidal anti-inflammatory drugs (NSAIDs such as ibuprofen), GLP-1 agonists (for diabetes and weight loss), antibiotics, and estrogens. Other medications that may cause indigestion include bisphosphonates, blood pressure medications, and certain supplements.
When to Seek Medical Attention
While mild, occasional indigestion is usually nothing to worry about, certain symptoms warrant prompt medical evaluation:
Consult Your Healthcare Provider If:
- Indigestion persists for more than two weeks despite lifestyle changes
- Symptoms are severe or worsening
- You experience unintentional weight loss or loss of appetite
- You have difficulty swallowing that progressively worsens
- You notice signs of anemia (fatigue, weakness)
Seek Immediate Medical Care If You Experience:
- Chest pain that radiates to the jaw, neck, or arm
- Shortness of breath or sweating along with chest discomfort
- Severe abdominal pain
- Vomiting blood or material that looks like coffee grounds
- Black, tarry stools (indicating possible internal bleeding)
The symptoms of severe indigestion or heartburn and a heart attack can be very similar. If you’re uncertain, it’s always better to err on the side of caution and seek emergency care.
Diagnosis: What to Expect
If you consult a healthcare provider about persistent indigestion, they will typically begin with a thorough medical history and physical examination. This may be sufficient if your symptoms are mild and you don’t have concerning warning signs.
However, if symptoms began suddenly, are severe, or you’re over 55 years of age, your provider may recommend:
Laboratory Tests: Blood work to check for anemia, thyroid issues, or other metabolic disorders.
H. pylori Testing: Testing for H. pylori is commonly done if you have frequent bouts of dyspepsia. This can be performed through stool samples or breath tests.
Endoscopy: A procedure where a thin, flexible tube with a camera is passed down your throat to examine your upper digestive tract. Tissue samples may be taken for analysis.
Imaging Studies: X-rays or CT scans to check for intestinal obstruction or other structural issues.
Effective Treatment and Management Strategies
The good news is that most cases of indigestion respond well to lifestyle modifications and, when necessary, medication. Treatment depends on the underlying cause and severity of symptoms.
Dietary Modifications
Diet plays a major role in controlling acid reflux symptoms and is the first line of therapy used for people with GERD.
Foods to Avoid or Limit:
- Fatty, fried, and greasy foods
- Spicy dishes
- Citrus fruits and tomatoes
- Chocolate
- Caffeine and carbonated drinks
- Alcohol
- Peppermint (despite being popular, it can actually worsen symptoms for some people)
Foods That May Help:
- Whole grains (oatmeal, brown rice, whole wheat bread)
- Lean proteins (chicken, fish, turkey)
- Green vegetables and root vegetables
- Non-citrus fruits (bananas, melons, apples)
- Low-fat dairy products
- Ginger and fennel
Research indicates that fiber-rich diets may be particularly beneficial. Research shows that people with high-fiber diets experience fewer acid reflux symptoms than those with low-fiber diets.

Eating Habits That Make a Difference
How you eat is just as important as what you eat:
Eat Smaller, More Frequent Meals: Smaller meals are easier on your stomach because they put less pressure on the valve that connects your esophagus and stomach.
Slow Down: Chew food thoroughly and eat at a relaxed pace. It takes 15-20 minutes for your brain to register fullness, so eating slowly helps prevent overeating.
Time Your Meals: Stop eating at least 2-3 hours before lying down or going to bed. This allows time for your stomach to empty before you recline.
Stay Upright After Eating: Avoid lying down immediately after meals. If you need to rest, try propping yourself up or taking a gentle walk instead.
Create a Calm Eating Environment: Care should be taken to create a calm and relaxed atmosphere, eat in small quantities, and chew the food slowly and completely.
Lifestyle Changes
Elevate Your Head While Sleeping: Raise the head of your bed 6-8 inches using blocks or a wedge pillow. This uses gravity to help keep stomach contents where they belong.
Maintain a Healthy Weight: Excess weight, especially around the abdomen, increases pressure on your stomach and can worsen symptoms.
Quit Smoking: Tobacco use weakens the lower esophageal sphincter and increases acid production.
Manage Stress: When indigestion is a result of stress, stress management techniques such as counseling, relaxation exercises, meditation practices such as yoga, and deep breathing are considered useful.
Review Your Medications: Talk to your doctor about any medications you’re taking that might be contributing to indigestion. Don’t stop prescribed medications without medical guidance.
Medical Treatments
When lifestyle changes aren’t enough, several medication options are available:
Antacids: Over-the-counter options that neutralize stomach acid for quick relief. Best taken when expecting symptoms.
H2 Receptor Antagonists: Reduce acid production and provide longer-lasting relief than antacids.
Proton Pump Inhibitors (PPIs): Powerful acid-reducing medications typically prescribed for more severe or persistent symptoms.
Prokinetics: Medications that help your stomach empty faster, useful for delayed gastric emptying.
Antibiotics: If H. pylori infection is detected, a combination of antibiotics will be prescribed to eradicate the bacteria. A recent systemic review and meta-analysis of 29 studies published in 2022 suggests that successful treatment of H. pylori modestly improves indigestion symptoms.
Living With Indigestion
For those dealing with chronic or recurring indigestion, keeping a food and symptom diary can be invaluable. Track what you eat, when you eat, your activities, stress levels, and any symptoms that occur. Over time, patterns may emerge that help you identify your specific triggers.
Remember that managing indigestion is often a process of trial and error. What works for one person may not work for another, and you may need to experiment with different strategies to find what provides relief.
The Bottom Line
Indigestion is a common digestive complaint that can significantly impact your quality of life. While occasional episodes are normal and usually harmless, persistent or severe symptoms deserve medical attention to rule out underlying conditions.
The good news is that most cases of indigestion can be effectively managed through a combination of dietary changes, lifestyle modifications, and when necessary, appropriate medication. By understanding your triggers, making strategic adjustments to your eating habits, and working with your healthcare provider, you can find relief and get back to enjoying your meals without discomfort.
With no definitive cause or cure, functional dyspepsia can be a frustrating diagnosis for people looking for answers. However, with patience and persistence in identifying what works for your body, most people can achieve significant improvement in their symptoms and overall digestive comfort.
If you’re struggling with frequent indigestion, don’t hesitate to consult with a healthcare provider. Early intervention can prevent complications and help you develop an effective management plan tailored to your specific needs.
Sources:
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK)
- Cleveland Clinic
- Johns Hopkins Medicine
- Mass General Brigham
- Mayo Clinic
- Medical News Today
- WebMD
- Patient.info
- International Foundation for Gastrointestinal Disorders (IFFGD)
- Various peer-reviewed medical journals and systematic reviews